
Niger J Paed 2014; 41 (4): 302 - 306
REVIEW
Jaja T
Clinical characteristics of
Yarhere IE
children and adolescents with
thyroid disorders seen at the
University of Port Harcourt
Teaching Hospital: A five year
review
DOI:http://dx.doi.org/10.4314/njp.v41i4,2
Accepted: 17th June 2014
Abstract
Background Thyroid
dis-
13
years with male to female ratio
orders constitute a large proportion
1.7:1. Of the 18 children,
Jaja T
(
)
of
endocrine diseases in children
5(27.8%)
had
hyperthyroidism
Yarhere IE
and
adolescents. Diseases of the
Department of Paediatrics,
with a case of neonatal thyrotoxi-
University of Port Harcourt Teaching
thyroid have profound effect on
cosis, 10(55.6%) hypothyroidism
Hospital
metabolism, cognition, growth and
and 3(16.7%) euthyroidism. eight
Port Harcourt, Nigeria.
development in children. The pat-
(44.4%) had goiter. Nine (90.0%)
Email: tamunopriyej@yahoo.com.
tern of thyroid disorders in children
of
the children with hypothyroid-
in
our region is still under reported.
ism had congenital hypothyroid-
Objectives: To
describe the
clini-
ism with two cases of transient
cal characteristics of children and
hypothyroidism. Mean age at diag-
adolescents with thyroid diseases
nosis of children with congenital
seen
over a 5 year period in a terti-
hypothyroidism was 9.81months.
ary
centre in Port Harcourt
Only 2(22.2%) with congenital
Methods: A
retrospective review
hypothyroidism presented before
of
all cases of thyroid disorders
the age of 3weeks, the mean dura-
seen in the Paediatric endocrinol-
tion of neck swelling before pres-
ogy clinic
of
the University of
entation of children with goitre
Port Harcourt Teaching Hospital
was 19.6months. One (5.6%) child
from January 2009 to December
had thyroid cancer. Initial wrong
2013.The
information
obtained
referrals and lost to follow up in
from endocrine registers and case
22.2% of cases each were common
files were patients’ biodata, clinical
challenges encountered in manage-
features, diagnosis, management,
ment.
challenges and outcome. Diagnosis
Conclusion: Congenital
hypothy-
of
each disorder was based on
roidism was the commonest thy-
clinical features, relevant labora-
roid disorder in this report, delayed
tory investigations and imaging
diagnosis and its consequences
studies.
were noted, emphasizing the need
Result: Eighteen
(29.3%) out
of
for routine new-born screening in
62
children with various endocrine
Nigeria.
disorders had thyroid diseases,
accounting for 0.1% of all children
Keywords:
Thyroid
disorders,
seen in the specialist outpatient
children, endocrine diseases, anti-
clinics. Age range at presentation
thyroid treatment
of
children reported was 5days to
Introduction
Disorders of thyroid function in children as in adults
manifest as hypothyroidism, hyperthyroidism and vary-
Thyroid disorders constitute a large proportion of endo-
ing degree of thyroid gland swelling (goitre) or a combi-
nation of these . The frequency of thyroid disorders
3
crine disorders in childhood. It is the second commonest
endocrine disorder after diabetes mellitus in children
varies from region to region with higher frequency in
worldwide . The importance of thyroid disorders in chil-
1
Iran, India and Bangladesh and lower frequency in La-
tiva however, this condition is recorded worldwide . In
4
dren is due to the profound effect of thyroxine on
metabolism, cognition, growth and development .
2
Nigeria, most studies on thyroid disorders were done in

303
Definitions of Terminologies
11
adults. There are only few but old reports mentioning
thyroid diseases in children . The prevalence of thyroid
5,6
disorders in children range from 0.07 -1.7% and fre-
Hyperthyroidism is
the production
and secretion
of
quency appears to be increasing . In the report by Ladi-
3
excessive amount of thyroid hormone (Triiodothyronine
tan et al in 1979, in the University College Hospital
T3
and/ or Thyroxine T4) from the thyroid gland with
Ibadan, the prevalence of thyroid diseases in children
high serum hormone levels.
was 0.07% and three decades later, a higher prevalence
Thyrotoxicosis: is
the hyper
metabolic clinical
syn-
of
0.12% was recorded in Benin City by Onyeruika and
drome that occurs when there is elevated serum level of
colleagues . In an earlier report on pattern of endo-
3,5
T3
and/or T4 irrespective of source of thyroid hormone.
crine diseases in Port Harcourt by Anochie etal col-
Hypothyroidism is the reduced production and secretion
leagues , thyroid diseases accounted for 13.3 % of all
of
T3 and/ or T4 from the thyroid gland with low serum
endocrine diseases . In Africa, iodine deficiency is the
7
hormone levels
commonest cause of thyroid disorders in both adults and
Hypothyroidism :
Is the
reduced production
and secre-
children . The UNICEF, estimates that 8% of newborn
8
tion of T3 and / or T4 from the thyroid gland with low
from Sub Saharan Africa are unprotected from learning
serum hormone levels.
disabilities resulting from iodine deficiency related dis-
Euthyroidism: is
a state
of normal
production and
se-
orders .
8
cretion of T3 and T4 from a thyroid gland with normal
serum hormone levels.
Presentation of thyroid diseases in children depends on
Goitre: This
is the
presence of
swelling in
front of
the
the age and geographic region. In infancy, congenital
neck due to thyroid gland enlargement with or without
hypothyroidism caused mainly by thyroid dysgenesis is
abnormality in T3 and/or T4 hormone production
a
common presentation diagnosed from new-born
Data was entered into an excel sheet and analysed using
screening or due to presentation with mental retardation
descriptive statistics and presented in text and tables
and
short stature during childhood. In later childhood
and
adolescence, asymptomatic goitre with autoimmune
disorders is commonest with a female preponderance .
9
In
most developing countries, iodine deficiency account
Result
for
the commonest cause of thyroid disorders ranging
General Description
from
congenital hypothyroidism to goitre in older chil-
dren
. The purpose of this study is therefore to describe
10
Eighteen (29.3%) out of 62 children with various endo-
the clinical characteristics of children and adolescents
crine disorders had thyroid diseases and were reviewed
with thyroid disorders seen in the Paediatric endocrinol-
accounting for 0.1% of total cases seen in the paediatric
ogy clinic of the University of Port Harcourt Teaching
specialist clinics. Age range at
presentation of chil-
Hospital over a five year period.
dren reported was 5days to 13 years with mean age of
72.9months. Nine (50%) of the patients were below five
years. There were 11 (61.1%) males and M: F of 1.7:1.
Of
the 18 children with various thyroid disorders, 5
Subjects and Methods
(27.8%) had hyperthyroidism with a case of neonatal
thyrotoxicosis, 10(55.6%) hypothyroidism and 3(16.7%)
The study was carried out in the endocrinology unit of
euthyroidism as in. Table 1. Overall, eight (44.4%) pa-
the department of Paediatrics, University of Port Har-
tients had goitre. Table 2 shows the general characteris-
court Teaching Hospital. The endocrine unit was started
tics of children with various categories of thyroid disor-
in
2001 as joint Nephrology/ Endocrine unit and became
ders.
an
independent unit in March 2013 with paediatric endo-
crinologist. The unit treats children and adolescents with
Table 1: Pattern
of Thyroid
Disorders in
Children Studied
various endocrine diseases. Children are referred from
Disorders
Male
Female
Total (%)
various private and government hospitals in Rivers State
and neighbouring states like Bayelsa, Imo, Abia and
Euthyroidism
1
2
3 (
16.7)
Akwa-ibom.
Hypothyroidism
8
2
10
(55.6)
Hyperthyroidism
2
3
5
(27.8)
Total
11(61.1%)
7
(38.9%)
18
(100%)
A
retrospective review of all thyroid cases seen over five
year period 2009 to 2013 was done. Information about
Hypothyroidism: Ten
(55.6%) patients
had hypothy-
the cases was retrieved from endocrine register, clinic
roidism out of which 9(90%) had congenital hypothy-
and ward records and case notes. Information on age,
roidism. Mean age at diagnosis of children with con-
sex, clinical features and duration of symptoms, diagno-
genital hypothyroidism was 9.81months. Of the nine
sis, treatment and outcome were retrieved. Diagnosis of
patients with congenital hypothyroidism 2(22.2%) cases
thyroid disorders was from clinical features, confirma-
had transient hypothyroidism. Two (22.2%) children
tory thyroid function test, antibody and histopathology
with congenital hypothyroidism were diagnosed by the
test.
age of 3weeks. Only one child (10%) an 11 year old
who was being investigated for short stature with cold
intolerance and constipation had acquired hypothyroid-
ism. In children with permanent congenital hypothyroid-
304
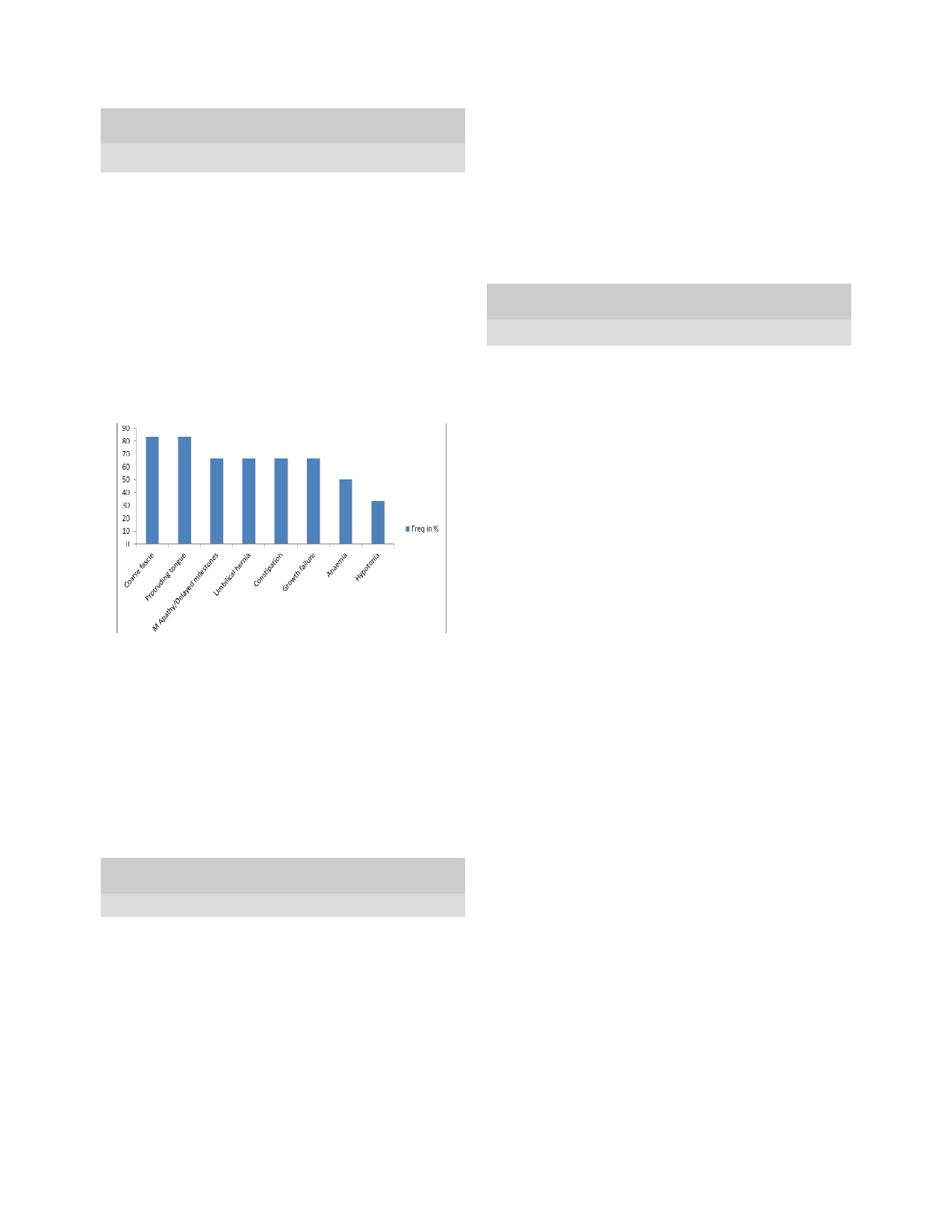
ism,
coarse fascie, protruding tongue and mental apathy/
19.6months. Challenges and outcome in children with
delayed milestone were the commonest features as
various thyroid disorders is as shown in Table 4. Infor-
shown in Fig 1.
mation was retrieved from documentations on patient’s
Table 2: Characteristics
of patients
with various
thyroid dis-
case
note and endocrine register during counseling sec-
orders
tions on treatment at clinic visits. Four (22.2%) contin-
Characteristics
Euthy-
Hypothy-
Hyperthyroid-
ued
to express worry over the prolonged use of the
roidism
roidism
ism
drugs. Four patients which included two children with
Number of Patients
3
10
5
Euthyroid goitre, the child with acquired hypothyroid-
Mean
age at presenta-
10.67year
22.07months
11
years
ism and one male with congenital hypothyroidism were
tion
s
(excluding
neonate with
lost to follow up. Only one, the child with the thyroid
Graves Dis-
cancer died giving a disorder -specific case fatality rate
ease)
of
5.6 %.
Age
range at presenta-
9-12
years
19
days -11
6weeks- 13
tion
years
years
Table 4: Challenges
and outcome
in management
of children
M:F
1:2
4:
1
2:3
reported
Mean duration of symp-
19.6
11.27months
12.8months
Challenges/Outcome
Freq (%)
toms at presentation
No
with Goitre
3
1
5
Initial wrong referral
4(22.2)
Difficulty doing baseline investigations
2(11.1)
Fig 1: Clinical
features in
children with
congenital hypothy-
Poor drug compliance
3(16.7)
roidism
Concern for prolonged drug therapy during counseling
4(22.2)
Lost to follow up in last 1 year
4(22.2)
Death
1(5.6)
Discussion
The prevalence of thyroid disorder in this study is 0.1%.
It
contributes to a significant proportion of paediatric
endocrine disorders seen in our centre. This prevalence
is
similar to a report of 0.12% by Onyeruika and col-
leagues in Benin City Edo State but it is 1.4 times
3
higher than a report by Laditan in University College
Hyperthyroidism: Table
2 shows
the general
character-
Hospital (UCH) Ibadan that was done three decades
ago . The higher prevalence reported in this study, com-
5
istics of children with hyperthyroidism. All children
with hyperthyroidism except one child with neonatal
pared to the report by Laditan in UCH may be due to
Graves’ disease presented between the age of 9 years
better awareness of the disease condition compared to
and
13 years. Soft goitre grade II to III, weight loss and
three decades ago when the study was done in UCH and
proptosis were the commonest reasons for presentation
also due to better access to specialist health care now.
however, the commonest clinical features of thyrotoxi-
cosis recorded at admission were weight loss, excessive
In
contrast to most reports on thyroid disorders in chil-
sweating and goitre seen in 100% of the cases as shown
dren and adults, this report found thyroid disorders was
in
Table 3. All children with hyperthyroidism were
1.7 times commoner in males. In the study by Onyeruika
and colleagues , it is four times commoner in females;
3
treated for Graves’ disease.
similarly, Ogbera and Kuku reported it was five times
commoner in adult females . The reason for a higher
8
Table 3: Frequency
of symptoms
at presentation
in children
with hyperthyroidism
number of males with thyroid diseases in this report is
Features
Frequency (% )
not very clear and calls for a need to carry out a larger
population study to confirm this finding.
Weight Loss
5(100)
Excessive sweating
5(100)
Goitre
5(100)
Thyroid disorders in children can present at any age,
Proptosis
4(80)
previous studies have shown that majority present dur-
ing
adolescence
3,8,9
Frequent Stools
3(60)
.
Onyeruika in his study in Benin
Poor Sleep
3(60)
reported a mean age of 11.2 years. This is however in
Palpitations
1(20)
contrast to the finding in this study where the mean age
Family History
1(20)
at
presentation of the children studied was 6.1 years
(72.3months). This was similar to the report by Laditan
in
1979 in UCH who noted a mean age of 5.4 years .
5
Euthyroidism: Three
(16.7%) children
were euthyroid
at
presentation,
mean
age
at
presentation
was
This reported younger age at presentation in this study
10.67years. The three children with euthyroidism pre-
and that by Laditan may be due to the fact that 50 to
sented with goitre (grade III) firm to hard lobulated goi-
60% of children reported in this study and that by Ladi-
tre out of which one had papillary thyroid cancer. Mean
tan had congenital hypothyroidism and most presented
duration of neck swelling before presentation was
before the age of 5 years.

305
The
expanding spectrum of thyroid diseases in children
Graves’ disease mother who presented with weight loss
and
adolescents includes three important clinical catego-
despite voracious appetite. He received carbimazole
ries
i.e. hypothyroidism, hyperthyroidism and euthyroid-
tablets transiently for three months and is presently on
ism.
The commonest disorder in this report was hypo-
follow up. The commonest reason for presentation of the
thyroidism accounting for half of all cases seen; which
patients with Graves’ disease was goitre and proptosis.
is
in contrast to the report by Onyeruika and colleagues
3
Features of thyrotoxicosis were reported in all children
in
Benin Southern Nigeria where hypothyroidism ac-
with
hyperthyroidism similar to reports from other studi-
es
3,18
counted for 22.2% of all cases of thyroid disorders seen
,
however; in children unlike in adults cardiovas-
cular complications such as heart failure is rare
3,18
over
a seven year period but similar to a report from
.
Singapore, and earlier report by Laditan in UCH where
hypothyroidism accounted for 40% and 60% of cases
Two subjects presented with euthyroid goitre, account-
of
thyroid disorders in children respectively
5,12
.
In an-
ing for 28.6% of all cases of goitre in this report. One of
other report from Mumbai, Northern India, hypothyroid-
the
cases with euthyroid goitre was suspected to have
ism
accounted for 75% of cases reported in children in a
chronic lymphocytic thyroiditis (CLT) which is the
referral centre . The differences in these rates may be
13
commonest cause of acquired thyroid disorder in chil-
accounted for by genetic and environmental factors of
dren with an initial preservation of thyroid function as
was recorded in this subject.
2,
9
which iodine deficiency may contribute. Iodine defi-
About 75% of cases of
ciency disorder is a common risk factor for thyroid dis-
CLT
are Thyroid peroxidase antibody positive, though
eases including congenital hypothyroidism. The high
this
could not be done before patient was lost to follow
number of children with CH in this report although can-
up.
The second case of goitre with normal thyroid func-
not
directly be attributed to iodine deficiency related
tion
was the patient with thyroid cancer which was diag-
disorders but it is important to note that in spite of the
nosed by a fine needle aspiration biopsy. Thyroid cancer
success in salt iodization and the availability of iodine
is
rare in children but is the second commonest malig-
rich
foods such as periwinkle, oysters and water in this
nancy in children exposed to radiation, Hodgkin’s lym-
phoma
and leukemia survivors . It also occurs in pa-
9
region, there is a rising incidence of endemic goitre
tients with existing chronic lymphocytic thyroiditis .
9
amongst the populace . This rising incidence of en-
14
demic goitre have been attributed to disorders of iodine
The
patient with thyroid cancer did not have any family
metabolism caused by food ,water and soil pollution
history of cancer and died in theatre during surgery.
from oil exploration as obtains in Port Harcourt .
14
Several management challenges were noted in this re-
The second commonest thyroid disorder in this report
port. These challenges include high cost and non-
was hyperthyroidism, which accounted for 27.8% of all
availability of investigations. In most cases, individual
cases. This finding is much lower than the report by
hormone profiles are expensive and are done by only
Onyeruika and colleagues who reported 67% of cases .
3
few laboratories. There is non– availabity in our centre
The difference in the rate between these studies is not
of
facilities such as thyroid scintigraphy needed to deter-
immediately obvious but may be due to environmental
mine actual cause of thyroid disease such as in congeni-
influences such as iodine consumption, diet and preva-
tal hypothyroidism or to exclude a toxic thyroid nodule
lence of endocrine disruptors. The possible reason for
in
children with hyperthyroidism. In this report, as in
the high rate of hyperthyroidism in the Benin study as
other reports low awareness both in the general populace
speculated by Onyeruika and colleagues may be due to
and even amongst health workers has been demon-
exposure to increased levels of iodine following the salt
strated; wrong referrals by health workers was noted in
iodization policy by the Government. The increased risk
children with proptosis who were wrongly treated for
of
hyperthyroidism following exposure to iodine has
eye disorders and referred to the ophthalmologist. Also
been reported in some studies
15,16
,
although no evalua-
the parent of a child with congenital hypothyroidism
who presented as early as 3 month of life with worry
rd
tion was done to determine the part of iodine levels in
children with hyperthyroidism in this study, however
over the dull disposition of the baby when compared to
Madukosiri in a pilot study on aetiology of goitre in
other babies was only reassured until the child was di-
Bayelsa State cautioned that the presence of iodine defi-
agnosed at age of 11 months. The delay in diagnosis of
ciency should be established in iodine replete areas be-
most of the children with congenital hypothyroidism and
fore salt iodization to prevent the excessive exposure of
presentation with mental retardation as was noted in this
the thyroid gland to iodine and its consequences such as
study was also reported in other studies, due to non-
increased thyroxine production .
14
availability of routine newborn screening. About a quar-
ter of the patients were lost to follow up in this report
In
this report all children with hyperthyroidism were
and this is not surprising as this is the pattern in our en-
treated for Graves’ disease an autoimmune disorder of
vironment in most chronic illnesses as parents tend to
the thyroid gland that results from complex genetic traits
seek alternative treatment. These challenges were also
noted in other studies
3,5,19
that occur in genetically predisposed individuals, it ac-
done in other centres stressing
counts for 60 -70% of cases of hyperthyroidism in pae-
the need for creation of awareness even amongst health
diatric age . Graves’ disease as in most other reports
17
workers.
was the commonest cause of hyperthyroidism in this
report with a female preponderance. One of the children
with hyperthyroidism was a neonate, an infant of
306
Conclusion
increase in children with mental retardation arising from
this. There is therefore the need for commencement of
Thyroid disorders are prevalent amongst children in Port
routine neonatal screening for congenital hypothyroid-
Harcourt adequate management is still hindered by lack
ism in our country and creation of awareness on thyroid
and high cost of diagnostic facilities. The commonest
disorders and other endocrine disorders.
disorder in this report was congenital hypothyroidism.
Delay in diagnosis of children with congenital hypothy-
Conflict of interest: None
roidism is still a major concern with a cumulative
Funding: None
References
5.
Laditan AAO, Johnson AOK. Thy-
1.
Becker KL, Nylen ES, Snider RH.
roid gland disorders in African
12.
Siok HT, Hock BW. Review of
Endocrinology and the endocrine
Children. J
Natl Med
Assoc. 1979;
thyroid Disorders in Singapore
patient. In: Becker L, Ronald CK,
71(2): 139-141
Children. J
Trop Pediatr1985;31
Rebar RW. eds, Principles and
6.
Edino ST, Mohammed AZ,
(1):54-58
practice of endocrinology and
Ochicha O, Thyroid diseases in
13.
Desai MP. Disorders of Thyroid
metabolism. 3 ed Lippincott,
rd
Kano. Niger
Postgrad Med
J.
gland in India. Indian
J Pediatr,
Williams and Wilkins, 2002: 82-
2004;11:103-106
1997;64(1):11-20
85.
7.
Anochie IC, Opara I, Inimgba N.
14.
Madukosiri CH. Delange F, de
2.
Desai MP.2009. Disorders of thy-
Pattern of endocrine diseases in
Benoist B, Alnwick D. Risks of
roid gland. In: Pathasarathy A, ed.
children in the University of Port
iodine- induced hyperthyroidism
I A
P Textbook of Pediatrics, 4
th
Harcourt Teaching Hospital. Port
after correction of iodine defi-
ed.
New Delhi, Japee Brothers
Har count Med J 2009;3:145-152
ciency by iodized salt. Thyroid
Medical Publishers Ltd, 931-935
8.
Ogbera AO, Kuku SF. Epidemiol-
1999;9:545-556.
3.
Onyiruika AN, Abiodun PO, Ony-
ogy
of thyroid diseases in Africa.
15.
Nte A, Idiki Ogan M, George I.
iruika LC. Thyroid Disorders in
India J Endocrinology 2011;5(6):
Paediatric thyroid gland disorders
Childhood and Adolescence:
82-88
in
Port Harcourt: Has the universal
Analysis of clinical data and man-
9.
Brown RS. Disorders of thyroid
salt iodization programme any
agement challenges in patients
gland in infancy, childhood and
role? TNHJ
2005;5:283-286
seen in a Nigerian Teaching Hos-
adolescence. Available at:
16.
Menon PS, Singh GR. Hyperthy-
pital. Greener
J Med
Sci 2012;
2
www.thyroidmanager.org.
roidism in children: an Indian ex-
(2): 045-050
10.
Fisher D. Next generation newborn
perience. J
Pediatr Endocrinol
4.
Rendon-Macias ME, Morales-
screening for congenital hypothy-
Metab 1996; 9: 441-446.
Gracia I, Huerta- Hermandez E,
roidism? J
Clin Endocrinol
Metab
17.
Zimmerman D, Lteif AN. Thyro-
Silva-Batalla A, Villasis-Keever
2005; 90(6):3797-9.
toxicosis in children.
Endocrinol
MA.
Birth Prevalence of Congeni-
11.
La Frenchi S. Disorders of the
Metab Clin North Am 1998: 27;
tal
Hypothyroidism in Mexico.
thyroid gland In: Kliegman RM,
109-126.
Paediatr and Perinatal Epidemiol
Berhman RE, Jenson HB, Stanton
18.
Hanna CE, La Frenchi SH. Adoles-
2008;22(5): 478-485
BF
eds. Nelson Textbook of Paedi-
cent thyroid disorders. Adolesc
atrics 18 ed. Philadelphia, Saun-
th
Med. 2002; 13(1):13-15
ders Elsevier, pp2316-2340